1601006132 - LONG CASE
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
A 61 year old male, hailing from miryalaguda ,shepherd by occupation came with chief complaints of
1. Pain in abdomen since 10 days,
2. Fever since 2 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 10 days ago ,then he developed
1. Pain in abdomen
It was diffuse and dragging type , insidious in onset , gradually progressive, associated with shortness of breath , it was non radiating with no diurnal variations , and relieved by sleeping sideways
2.Fever
From 2 days ,Low grade ,continous associated with chills and rigor ,relieved on taking medication.
No History of Nausea, Vomitings , Loose stools, flatulence ,loss of weight decreased urine output, dysuria.
PAST HISTORY:
-He had yellowish discoloration of eyes 6 months ago.
- No history of diabetes mellitus, hypertension, tuberculosis, epilepsy.
PERSONAL HISTORY:
•He takes mixed diet
•Appetite adequate
•Bowel movements are irregular.
•Bladder movements are regular.
•He is a chronic alcoholic and takes 90ml/day since 30 yrs
•He is a chronic smoker and takes 20 beedis/day since 30 yrs.
FAMILY HISTORY:
-Not significant
TREATMENT HISTORY:
Took medication in local hospital 6 months back for jaundice.
GENERAL EXAMINATION
-The patient is conscious, and cooperative.
- He is well oriented to time, place and person.
- He is moderately built and moderately nourished.
-Examination was done after taking proper consent & in a well lit room after adequate exposure.
•Bulbar conjunctiva of left and right eye are yellow in color.
-Bilateral pedal edema ,pitting type, upto the level of ankle region
✓There is no Pallor, Clubbing, Cyanosis, Generalized lymphadenopathy.
VITALS
Temperature -he is afebrile (at present)
Pulse = 84 beats per minute, regular, normal in volume and character. There is no radio-radial or radio-femoral delay. The condition of the arterial wall is normal.
-Blood pressure = 120/70 mm of Hg in supine position
- Respiratory rate = 22 cycles per minute.
-Sp O2 :93% at room air
- JVP is normal
LOCAL EXAMINATION
Oral cavity : brown staining of teeth
GASTROINTESTINAL EXAMINATION :
On Inspection:-
✓Anterior abdominal wall
-Abdomen is symmetrically distended and flanks are full
-Umblicus is below the midposition between xiphisternum and pubic symphysis, Slightly everted with horizontal Slit .
- Abdomen skin is smooth and shiny
-All the quadrants are equally moving with respiration
-No venous prominence when examined both on sitting and standing position.
-No scars ,ulcers ,visible pulsations.
- No Scratch marks on the abdomen.
-No hernial swellings with and without cough impulse
✓ Posterior abdominal wall,
No scars , swellings, pulsations
On palpation
•Superficial palpation ,
- Localised tenderness in the right hypochondrium
- elastic consistency
- No rise in temperature,guarding and rigidity,thrills
•Deep palpation,
- Liver is tender ,smooth ,firm , regular margin, moving with respiration.
- Spleen , kidneys , urinary bladder are not palable
-Abdominal girth is 84 cms
On Percussion,
Liver span - 16 cms
No shifting dullness
On auscultation,
Bowel sounds are heard
No venous hum,bruit, friction rub.
RESPIRATORY EXAMINATION
Upper respiratory tract examination -
Nose: No deviated nasal septum, No nasal polyps
Pharynx : no post nasal drip , congestion
Inspection;
• Chest is symmetrical in ,Elliptical in shape
•Trachea appears to be Central (Trails sign -ve)
•Movements of chest equal on the both sides
•No Visible Pulsations, Swellings,engroged Veins, Scars & Sinuses
•No signs of use of accessory muscles of respiration.
Palpation
- No local rise of temperature
- Trachea is Central
- Respiratory movements are normal
- Chest Expansion 5cm (from 80-85cm)
- Transverse diameter 29cm
-AP diameter 24cm
- Vocal fermitus Decreased on Right side lower region
- Apex beat is palpable in 5th intercoastal space ,1 cm medial to mid clavicular line
- No palpable lymph Nodes
Percussion
✓Direct : resonant over clavicular,sternum.
✓Indirect :
✓Anterior. Right. Left.
Supraclavicular: Resonant. Resonant Infraclavicular: Resonant. Resonant
• Resonant note in second to sixth right intercostal space
• Resonant note from second to sixth left intercostal space
✓Stony dull note on the right seventh intercostal space
✓ Lateral chest wall
Dull note in the right InfraAxillary region
✓Posterior: Right Left.
Suprascapular: Resonant. Resonant
Interscapular: Resonant resonant
Infrascapular: Dull . Resonant
Auscultation:
Right. Left
•Supraclavicular. Normal. Normal
• Infraclavicular. Normal. Normal
• Mammary Normal. Normal
•InfraMammary. Decreased. Normal
• InfraAxillary. Decreased. Normal
• suprascapular. Normal. Normal
• Infra Scapular. Decreased Normal
• Interscapular. Normal. Normal
CARDIOVASCULAR EXAMINATION
S1 S2 heard
No murmurs
Apex beat felt on 5th intercostal space
CNS
Higher mental functions are intact
No focal deficits seen
INVESTIGATIONS :
Complete blood picture
Complete urine examination
Liver function test
Ultrasound Abdomen
Aspiration of liver abcess
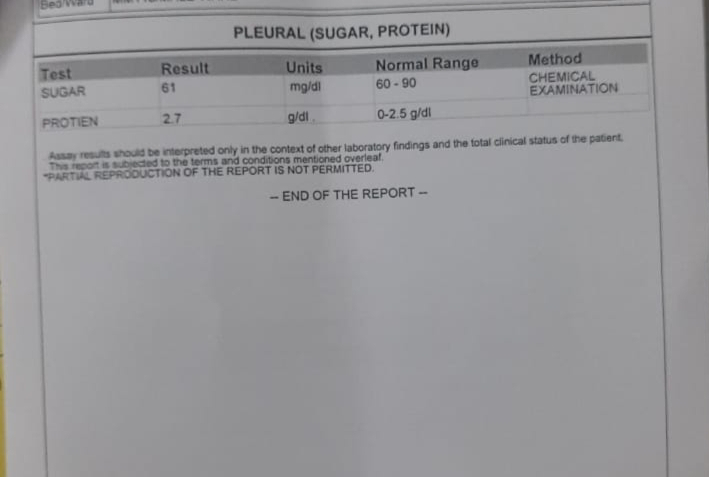
Pleural fluid examination
Pleural tap
CHEST X RAY
Abdominal X ray
ECG
Rate : 100bpm
Regular
Low voltage QRS complexes in L2 , AvF , V1
P waves T waves not visible in AvL
Left axis deviation
TREATMENT :-
1.INJ.MEROPENAM 500mg I.V ,BD
2.Inj.metrogyl 750mg I.V TID
3.Inj .pantop 40mg I.V,twice daily
4.Tab.Lasix 40 mg orally once daily
5 Tab.doxycycline 100mg oral twice daily
6.Tab.Linezoid 600mg per orally twice daily
7.Syrup lactulose 15 ml orally twice daily
8 Inj Vit.K 1 ampoule in 20ml .Normal saline I.V once daily
PROVISIONAL DIAGNOSIS :
Multiple pyogenic liver Abcess with right side pleural effusion.















Comments
Post a Comment