OSA
A 45 year old male driver by profession came with c/o
Snoring since 10 years
Excessive day time sleepiness since 10 years
Breathlessness episodes in sleep
He was apparently assymptomatic 10 years ago then he developed excessive day time sleeping and snoring which started affecting his daily activities
He is a known case of Hypertension and is on olmesartan 20 mg + amlong 5 mg since 8 years
Not a known case of DM,CVA,CAD,TB, EPILEPSY
PERSONAL HISTORY
Diet- mixed
Appetite - normal
Sleep- increased
Bowel and bladder movements - regular
Addictions- alcohol since 10 yrs weekly twice
Tobacco since 10 yrs weekly once
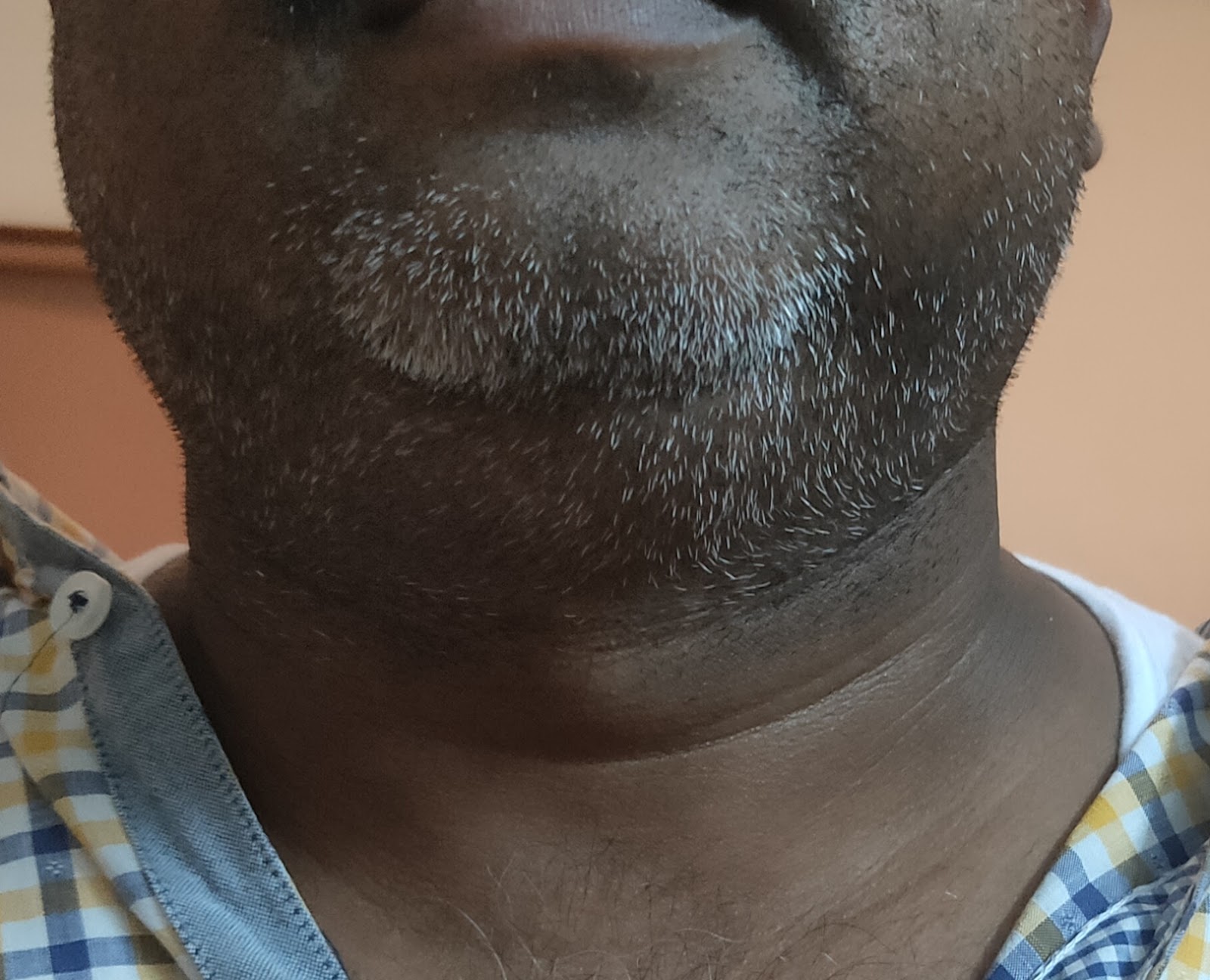
General physical examination
Pt is c/c/c
Moderately built and nourished
Temp- 98.6
Pr- 78 bpm
Rr- 18 cpm
Bp- 120/90 mm hg
Spo2- 99%
Grbs- 156 mg/dl
Systemic examination
Cvs- s1,S2 +
RS- bae+,nvbs
P/a - soft , nontender,bowel sounds +
Cns- nad
Provisional diagnosis- excessive day time sleepiness and snoring under evaluation
? OBSTRUCTIVE SLEEP APNEA
Investigations
Chest x ray
ENT REFERRAL
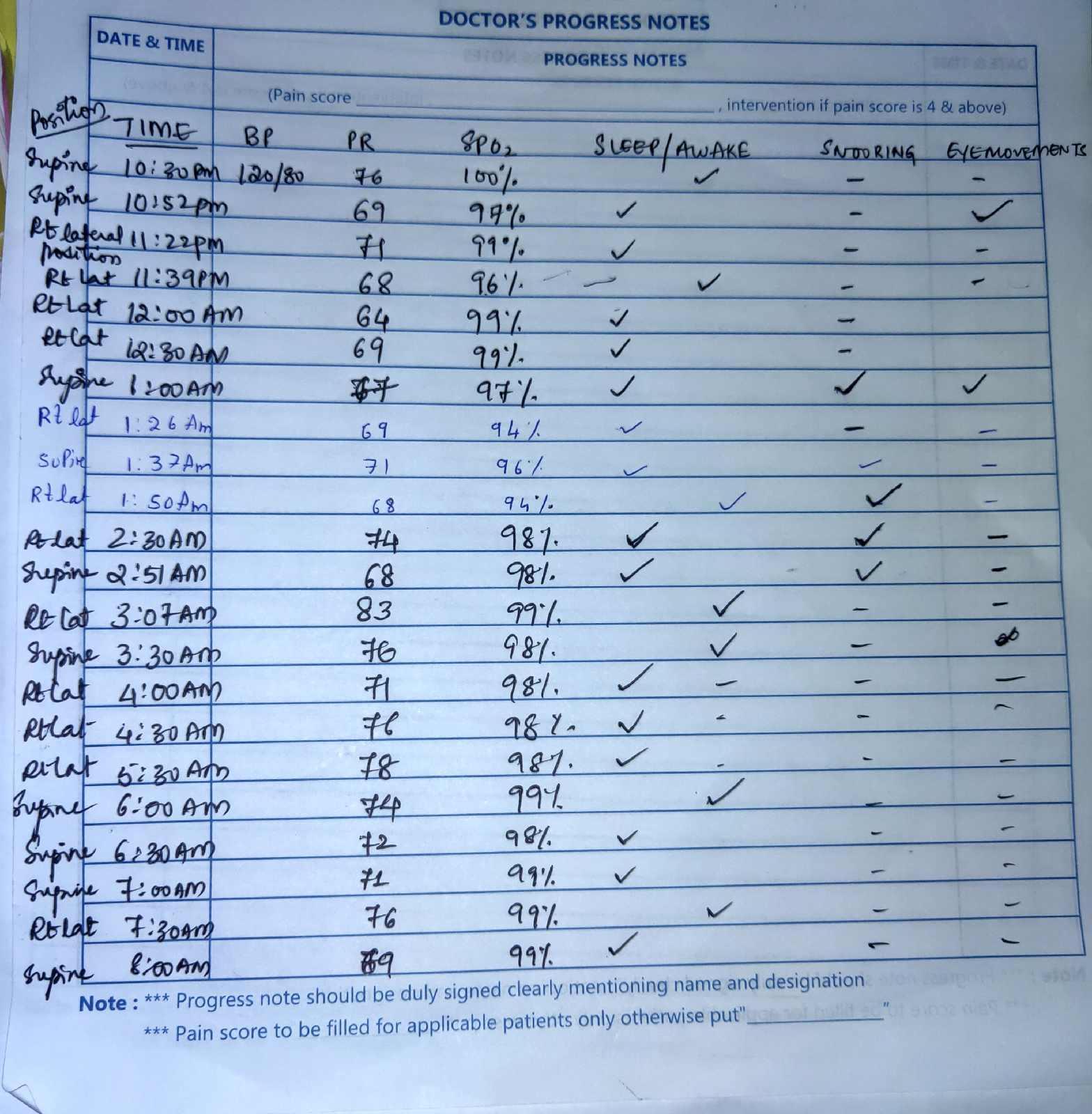
Night Monitoring day 1
Soap notes day 1
S- difficulty while sleeping,arousal+, awakening+, increased day time sleeping
O-
Temp- afebrile
Bp- 120/80 mm hg
Pr- 78 bpm
Cvs-s1,S2 heard
RS- BAE+
P/a- soft nontender,bowel sounds+
Cns- nad
A- obstructive sleep apnea
P-
bp/pr/spo2 monitoring during sleep
Tab.mvt po od
Soap notes day 2
S- patient feels better than yesterday ,had better sleep at night
O-
Temp- afebrile
Bp- 120/80 mm hg
Pr- 72 bpm
Spo2- 99%
Cvs-s1,S2 heard
RS- BAE+,nvbs
P/a - soft nontender
Cns- nad
A- obstructive sleep apnea
P
1.CPAP -overnight (during sleep)
2.tab.mvt po od
Monitoring during sleep day 2
No hypoxic epiodes with CPAP .
Without CPAP - max drop in spo2-86%
With CPAP - least spo2 was 94%
Snoring episodes - without CPAP -13
With CPAP -4
Awakenings -
Without CPAP - 4
With CPAP -7
Dental referral
DISCHARGE SUMMARY
A 45 year old male driver by profession came with c/o
Snoring since 10 years
Excessive day time sleepiness since 10 years
Breathlessness episodes in sleep
He was apparently assymptomatic 10 years ago then he developed excessive day time sleeping and snoring which started affecting his daily activities
He is a known case of Hypertension and is on olmesartan 20 mg + amlong 5 mg since 8 years
Not a known case of DM,CVA,CAD,TB, EPILEPSY
PERSONAL HISTORY
Diet- mixed
Appetite - normal
Sleep- increased
Bowel and bladder movements - regular
Addictions- alcohol since 10 yrs weekly twice
Tobacco since 10 yrs weekly once
General physical examination
Temp- 98.6
Pr- 78 bpm
Rr- 18 cpm
Bp- 120/90 mm hg
Spo2- 99%
Grbs- 156 mg/dl
Systemic examination
Cvs- s1,S2 +
RS- bae+,nvbs
P/a - soft , nontender,bowel sounds +
Cns- nad
Diagnosis-
OBSTRUCTIVE SLEEP APNEA
PLAN OF CARE
OVERNIGHT CPAP
MANDIBULAR ASSSIT DEVICE
Mechanism of action of MAD
MAD prevent upper airway collapse by protruding the mandible forward, thus altering the jaw and tongue position. They are also referred to in the literature as mandibular advancement splints (MAS) or mandibular repositioning appliances (MRA). Both video endoscopy and magnetic resonance imaging (MRI)-guided studies have determined that these devices predominantly increase the volume of the airway at the level of the velopharynx (11,12). The airway space is mostly enlarged laterally, thought to be due to traction on soft tissue connections between the pharynx and the mandibular ramus
Phillips et al. (29) showed that CPAP and MAD achieved similar improvements in EDS and QoL. Average MAD compliance was 6.5 hours/night compared to 5.2 for CPAP (P<0.0001). These results are consistent with other studies (23,24,32), supporting the hypothesis that MAD and CPAP have similar clinical effectiveness due to greater MAD compliance achieving net similar AHI reduction.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5803051/

















Comments
Post a Comment